Dissecting Prof. Muhammad Ali Pate’s Red Letter and NARD’s Impending Strike

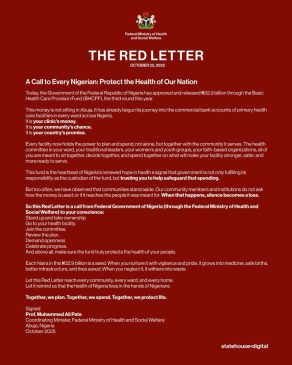
When the Federal Ministry of Health released The Red Letter on October 22, 2025, it seemed like a fresh breeze in a stifled room; I even posted it on my Twitter and Facebook accounts.
The letter, signed by Coordinating Minister of Health and Social Welfare, Professor Muhammad Ali Pate, called on Nigerians to “protect the health of our nation.” It announced the release of N32.9 billion through the Basic Health Care Provision Fund (BHCPF), the third disbursement this year, to primary health care centres across the country.
At first glance, the tone was progressive. It sounded like an inclusive call to action, urging citizens to take ownership of their local clinics and hold leaders accountable. But on closer examination, this “red letter” is both a mirror and a mask: a mirror reflecting the government’s awareness of the people’s distrust, and a mask concealing the structural decay that N32.9 billion cannot fix.
According to TrackaNG, the N32.9 billion is to be distributed among roughly 8,000 primary health care centres nationwide. That translates to just about N4 million per facility, barely enough to make a dent in the rot. To put it in perspective, N4 million can barely cover defibrillators for each centre, let alone cover drugs, electricity, water supply or building repairs amongst other things. The Math alone tells a grim story.
The letter claims that the funds have already begun their “journey into the commercial bank accounts” of health facilities. That phrasing should have reassured citizens, but instead it sparked scepticism. Transparency in Nigeria’s public sector remains elusive. Many Nigerians are wondering who exactly monitors these accounts, what procurement processes are in place, who sits on the committees overseeing spending, and how often reports are made public.
A 2024 survey by the Development Research and Projects Centre (DRPC) found that only about 61% of health professionals rated Nigeria’s health financing system as even “moderately functional,” while nearly 9% described it as “non-functional.”
That perception aligns with decades of under-funding. In the 2025 budget, the health sector accounted for only 5.15% of total government spending, far below the 15 per cent target set by African leaders under the Abuja Declaration. The World Bank also estimates that public health expenditure in Nigeria remains just about 3 per cent of GDP, one of the lowest in Sub-Saharan Africa.
The pageantry surrounding this release exposes a deeper malaise: that Nigeria’s health system is so chronically under-funded that routine budgetary disbursements now feel like national celebrations. In countries where healthcare is prioritised, such releases are bureaucratic normality. Here, they are headline events.
This latest government effort arrives at a perilous moment. The Nigerian Association of Resident Doctors (NARD) has announced that its members will begin an indefinite strike on Friday, October 31, 2025, citing unpaid allowances, decaying infrastructure, and unresolved welfare issues. Their grievances are not new. They echo years of neglect that have hollowed out public hospitals and driven thousands of skilled professionals abroad.
The irony is sharp. While the government is calling on citizens to “join committees” and “review plans,” the very backbone of healthcare, doctors, nurses and support staff, are either protesting, emigrating, or burning out. The National Association of Nigerian Nurses and Midwives reported earlier this year that over 75,000 nurses have left the country in the past five years.
The Nigerian Medical Association estimates that fewer than 25,000 doctors now actively practice in Nigeria, serving a population of over 200 million. That is roughly one doctor for every 8,000 Nigerians, compared to the World Health Organization’s recommended ratio of one to 600.
In major teaching hospitals, equipment failures are common. Diagnostic machines break down for months before repair. At primary health centres, simple tools like blood-pressure monitors or sterilisers are often missing. Many rural clinics have no running water, power, or basic delivery beds. It is hard to see how N4 million per facility can reverse such collapse.
The letter also raises questions about what kind of health system Nigeria seeks to build. The BHCPF is meant to strengthen primary care, but N4 million per facility is symbolic at best. When shared further among drugs, maintenance, and committee operations, what is left to transform service delivery?
Public reaction to The Red Letter has been mixed. Some Nigerians applauded the transparency of publishing such a message. Others saw it as political theatre, a glossy announcement masking deeper dysfunction. On social media, many expressed fatigue. After years of unmet promises, they are reluctant to celebrate what feels like routine governance dressed up as reform. That scepticism is a teachable moment for government. It reveals how profound the trust deficit between state and citizen has become. When people no longer believe in reform, even good intentions lose their power.
Professor Muhammad Ali Pate, to his credit, is a consummate professional. A former Minister of State for Health and a globally respected expert, he has served with the World Bank and led GAVI, the Vaccine Alliance. His credentials far outshine those of many before him. But being better than poor predecessors is not enough. The test of leadership is not professional pedigree but practical change.
The deeper problem with The Red Letter is that it romanticises community participation without confronting the structural dysfunction that makes such participation futile. Health committees cannot enforce accountability in an environment of opaque procurement, political interference, and chronic under-funding. Calling on citizens to “stand up” sounds inspiring, but standing up requires resources, institutional support, and trust, all of which are in short supply.
Meanwhile, health workers continue to earn salaries that make survival itself a challenge. Reports show that doctors earn between N350,000 and N500,000 per month, while consultants average around N1 million, figures that pale against the cost of living or what peers earn abroad. Nurses often take home less than N200,000 despite long shifts in ill-equipped wards. Without competitive pay, modern tools, and safe working conditions, Nigeria will keep losing its best minds.
The truth is that Nigeria’s healthcare system does not need more slogans. It needs sustained funding, transparency, and reform. It needs to modernise hospitals, equip rural clinics, and digitalise procurement to make every naira traceable. It needs to respect the professionals who sustain it.
The Red Letter should be more than a statement; it should mark the start of accountability. But for that to happen, government must move from symbolism to substance. Citizens, too, must go beyond cynicism and demand measurable transparency in how funds like the BHCPF are used.
Nigeria’s health, quite literally, depends on it.
Ndi Kato is a political analyst, commentator and gender advocate challenging the systems that shape governance and social progress.










